Glioblastoma, also known as glioblastoma multiforme (GBM), is the most aggressive and common type of malignant brain tumor in adults. It accounts for approximately 15% of all brain tumors worldwide, with up to 25,000 new cases diagnosed annually in Europe. This cancer originates in the glial cells and is characterized by its rapid growth and ability to infiltrate surrounding brain tissue, making it particularly difficult to treat. One of the main reasons for this difficulty is the induction of an immunosuppressive microenvironment (EMT) by the tumor cells, leading to immune escape. Within the EMT, several complex interactions occur among various cell types, notably the physical interaction between pericytes (PC) and tumor cells, which promotes angiogenesis, immunosuppression, and metastasis. Current treatments for GBM include surgery, radiotherapy, and chemotherapy but have significant limitations, highlighting the need for more reliable and effective treatments.
To address this challenge, researchers at the University of Murcia (Spain) have identified a new therapeutic target for the treatment of GBM based on the modulation of the EMT and have developed a cell therapy with genetically modified pericytes as a potential treatment for this disease.
The proposed technology relies on the use of genetically modified pericytes, insensible to tumor-induced alterations. This approach aims to enhance the anti-tumor functions of pericytes, thereby slowing or inhibiting tumor progression.
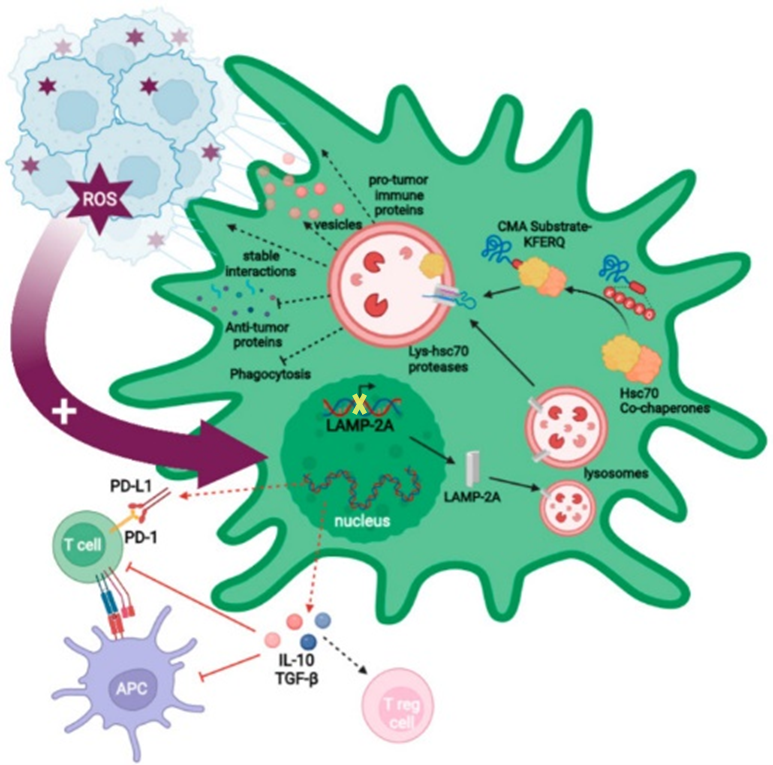
Specifically, these pericytes, which has been purified from vascular fraction of adipose tissue, are genetically modified without chaperone-mediated autophagy (CMA) pathway. This is achieved by genetically modifying them to inhibit the expression of or delete, the LAMP2A gene. This improves the anti-tumor immune response in the brain, eliminating tumor cells and preventing their dissemination to the brain.
The technology has demonstrated effectiveness in treating human GB cells through in vivo xenograft studies conducted in mouse models.
Benefits:
- It offers a unique and effective alternative for the treatment of GBM. It not only targets and eliminates tumor cells but also stimulates an antitumor immune response.
- By employing a personalized approach, it can adapt to individual patient needs, overcoming tumor resistance.
- It eliminates glioma cells without interacting with the host’s endogenous pericytes.
- This therapy has potential for extension to other cancers, particularly those resistant to current treatments.
The represented institution is looking for feedback from the industry and aims to establish a collaboration that leads to the commercial exploitation of the presented invention. The ideal scenario for the company would be to reach an agreement to transfer the technology by a license (exclusive or non-exclusive) of the patented procedure, or a co-development. However, the form, terms, and conditions of the collaboration can be openly discussed if the technology is of interest.
Institution: Universidad de Murcia and the Instituto Murciano De Investigación Biosanitaria (IMIB).
TRL: 3-4
Protection status: Patent application, extended internationally in Europe and the USA.
Contact: Elisa Sáenz / e.saenz@viromii.com

